HealthNxt: The Next Great Advance in Virtual Care


The HCI Group was pleased to welcome our Chief Medical Officer and expert in healthcare and technology, Matt Lambert. Matt is a practicing emergency medicine physician and has served in Interim CMIO and CMIO support roles for multiple health systems including New York City Health and Hospitals, Johns Hopkins, Medstar, and Inova. He possesses deep knowledge of current healthcare legislation and how it has impacted current healthcare environment and EMR marketplace. Dr. Lambert has a demonstrated ability to leverage new technology to facilitate new population health and risk adjusted reimbursement models. He is the author of two healthcare books: Unrest Insured and Close to Change: Perspectives on Change and Healthcare for a Doctor, a Town, and a Country. Matt joined Ed Marx, HCI’s Chief Digital Officer and former Cleveland Clinic CIO to take part in HCI’s in a webinar session to discuss the next great advance in virtual care: HealthNxt.
The Current State of Virtual Care
When asked about the current state of virtual care, Matt Lambert is excited by the changing landscape and sites a plethora of examples that show a tantalizing shift in an industry that has gained a reputation as stodgy when it comes to embracing the cutting edge in the treatment of patients. For example, Becker’s Hospital Review, a leading industry publication, estimates a 4,000 percent increase in telehealth claim lines from March 2019 to March 2020. Based on these numbers, experts predict a whopping one billion telehealth visits in 2020 alone. Reporting from various health organizations around the country would seem to corroborate this claim: NYU Langone Hospital estimates their telehealth visits are up 4300 percent; Atrium Health is reporting a 6000 percent increase in telehealth visits from last year; Novant reports that telehealth visits have gone from an average of 200 a year to 12,000 visits a week.
Matt believes that while this sudden pivot is due in large part to the COVID-19 pandemic, there is a great opportunity for the healthcare community to embrace virtual care as an integral part of the provider model.
“All of this was a pivot to treat COVID-19 patients or provide care in a way that minimized risk from a contagion. We think this is really opening an opportunity for [telehealth] to be a more integrated part of care.”
Furthermore, the COVID-19 crisis has helped to knock down the remaining barriers that were preventing healthcare providers from embracing a virtual care model. For instance, the Centers for Medicare and Medicaid has responded to the need for virtual care by introducing reforms such as the 1135 waiver, to effectively abolish the need for face-to-face interactions when dealing with medical claims and reimbursements. This reform allows these transactions to take place over any modality.
“I think [from a financial perspective] we are going to see [a shift] to more HIPAA-compliant platforms, but its created a lot of opportunity through crisis, and certainly bowled over the barriers that prevented many providers from adopting a more integrated model.”
Evolution of Virtual Care
According to Matt Lambert the new provider model will be a hybrid one. This could mean that up to 40 percent of provider-patient encounters are of the virtual kind.
“[Virtual care] isn’t going back in the bag. This is not only because of efficiency, but because I think a lot of patients and providers are going to enjoy [the virtual care] experience more. I think for existing patients, which is most ambulatory visits, I do not think we will see any compromise in quality at all. Physicians my age or younger rely so much on diagnostic technology to help us with diagnosis rather than more traditional observational methods. I do not think we are going to miss out on many critical findings. Providers will need to understand the limits of the technology and adjust the threshold for converting to in-patient visits accordingly.”
A shift toward virtual care can also help favor patients who deal with health and social equity issues. Providers would be able to deliver care to patients directly in their homes via the internet or over the phone, thus eliminating issues with timing due to work schedules or lack of adequate transportation. To make this model work, Matt foresees that significant investments need to be made in infrastructure—from improving network connectivity and availability to instituting community provisioning programs to help with outreach for elderly and immobile patients.
“The challenge from the social equity piece of this puzzle is that we are going to have to make some active investments at a community level. I think that there is a real opportunity to level the outcomes associated with those determinants.”
HealthNxt: The Next Step in Virtual Care
Beyond the financial reforms which have paved the way to our new normal, the shift to virtual care has forced both patients and providers to change their expectations of what a traditional care model might look like in the future. To this effect, Matt has been working with HCI’s parent company Tech Mahindra’s Health and Life Sciences (HLS) vertical to help develop the HealthNxt platform: an integrated, single enterprise platform with the capability to handle multiple functions throughout the virtual care spectrum from episodic care to longitudinal care. Furthermore, HealthNxt will seamlessly integrate EHR access, and remote patient monitoring and other tools and features to allow for a fully integrated inpatient experience at home.
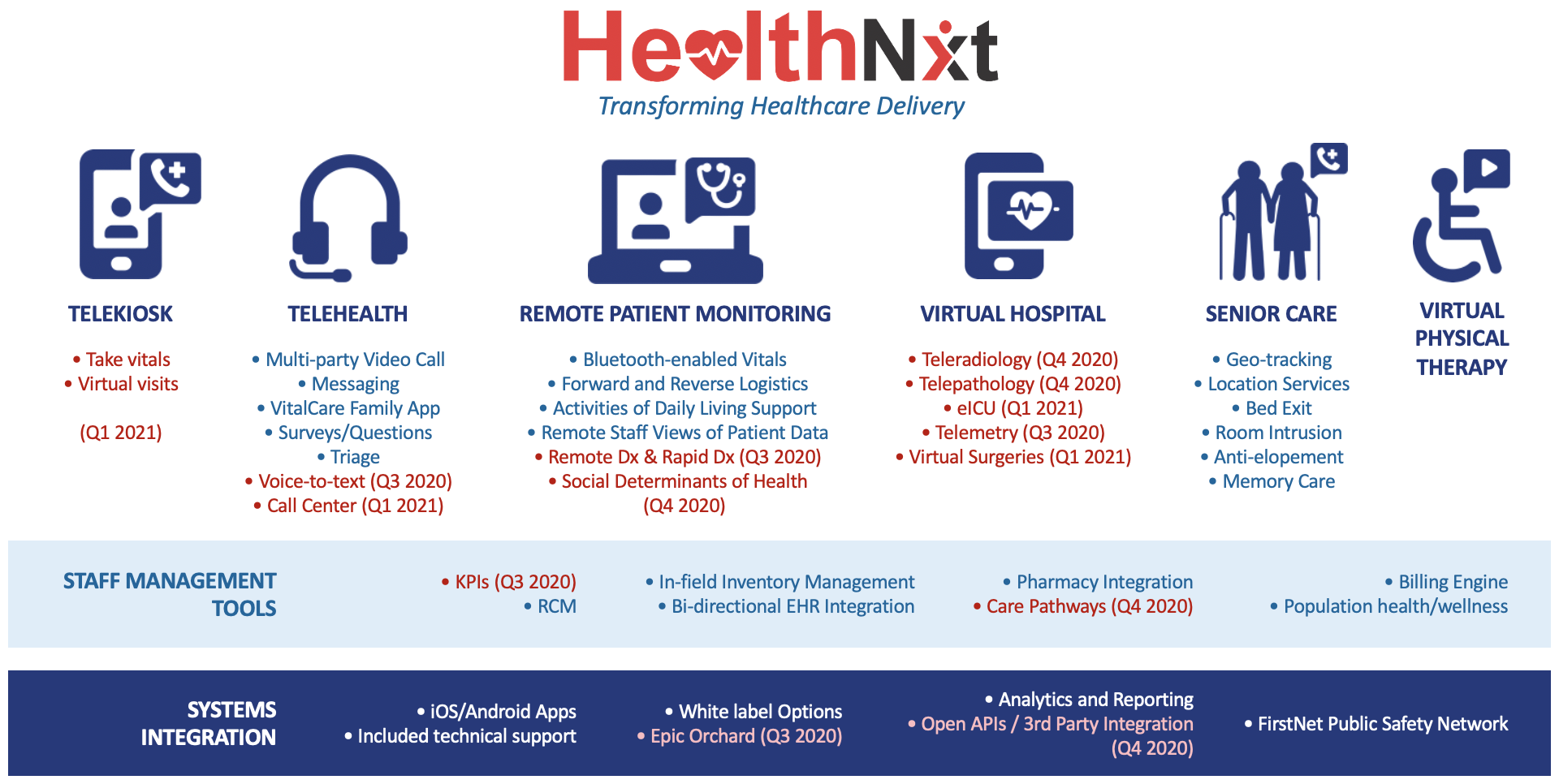
“There will be a shift from retail-focused, episodic care to more longitudinal care. This will place an emphasis on the relationship between providers and patients. The focus will be on integration on the enterprise level, not cobbled together with a variety of interfaces and licenses for different products. As we get more sophisticated an emphasis will be placed on population health. This means incorporating remote patient monitoring for at-risk and infirm populations to reduce potential readmissions and to help communities and healthcare organizations from a strategic level. Eventually I think this will evolve into hospital-level care provided at home, whether it be shortening the length-of-stay for certain diagnoses or whether it be inpatient-level care given from the beginning with remote patient monitoring. I think this is where we’ll see the virtual care model grow and expand 90 days from now and moving forward.”
