Fostering Collaboration and Addressing Implementation Challenges

The Need for a Collective Approach to Foster Collaboration and Address Implementation Challenges
In our NHS engagements, we encourage and facilitate open and transparent dialogue and coordination of best practice across NHS organisations to learn from each other's experiences. We believe that fostering this collaborative culture can lead to substantial cost savings and more informed decision-making processes. Each ICS and Trust can benefit from streamlining and sharing knowledge in their improvement plans.
Potential Challenges and Barriers:
We acknowledge that implementing this collective approach is likely to encounter some challenges if not barriers.
One such challenge could be overcoming the historical autonomy of individual Trusts and ICSs in decision-making processes. There may be reticence where the same senior roles exist across multiple organisations. Yet the NHS is sufficiently early-on in its data and digital evolution that there are nationally many gaps in leadership which could be filled through a redeployment of these decision makers. This rationalisation is not likely to happen without national leadership in resourcing strategy. Such rationalisation will break down silos and enhance organisational collaboration.
Another can be the existence of pockets of absence of experienced data and digital leadership or its inability to influence the Executive board. It can be difficult to persuade an oft Clinically led yet holistically inexperienced Executive board in how technical and digital foundations need to be in place to deliver clinical and operational improvements.
Another could be the varying levels of readiness and digital maturity across different Trusts and ICSs. Some might already have well-established EPR systems, while others may still rely on traditional paper-based processes. Integrating these disparate systems and aligning them towards a unified goal will present technical, operational and change management complexity.
Short case study
The purchase of an electronic patient record system (EPR) is a significant part of an individual Trust's system estate refresh. Yet HCI have experienced three out of three instances now where individual Trusts are choosing between EPR providers without a data strategy in place. The data strategy enables a Trust to consider the broader Trust as well as ICS data and digital enablement context. It also enables the Informatics department to ensure that all guidance published by NHS England is taken into account, such as separating the storage of data produced by the application from the application. And as a result of an absence of data strategy, and the weakness in technical leadership, clinical decision makers have been persuaded by the EPR vendors, that the EPR system can be and should be the home of the Trust’s entire dataset, endangering the optimal future set-up of their data to support their digital and clinical strategies. The clinical leadership has also been swayed into choosing some of the more expensive EPR vendors when some of the desired differentiating functionality could have perhaps been delivered from the addition of a vendor agnostic separate yet integrated data layer.
From a Trust perspective, a slightly less functionality rich EPR + data layer, which together as a system delivered all the desired functionality, may be a cheaper option than a more expensive top tier EPR and subsequently implemented data warehouse or set of broader EPR data integrations. From the perspective of the ICS, the goal of convergence and enabling interoperability within an ICS may be more easily attained. That only leaves the question about convergence and equity across ICSs. Does the use of certain EPRs or presence of certain functionality improve outcomes?
Recommendations addressing key observations
We would like to make a series of recommendations to contribute to open discussion which may already be happening. The data vision guidance required by every Trust and ICS is similar. However, its implementation needs to be dependent on localised assessment and strategy on how to move along the same journey:
- from different starting points in data capability and
- with different maturity of EPR system implementation.
- with different system estate refresh needs to support a Trust’s digital ambitions.
- with different strengths in relationships with regional Trusts and the ICS
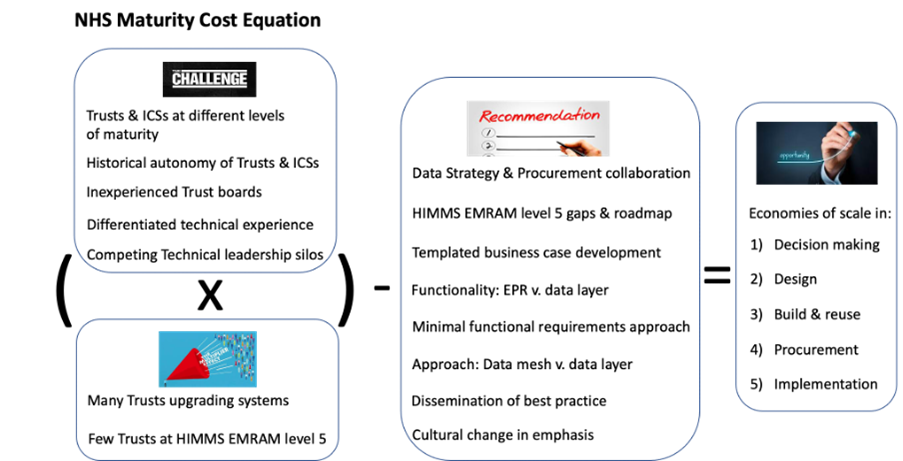
Recommendation 1: Encouraging collaboration in collective data strategy and procurement
Collaboration across individual Trusts within an ICS, and across ICSs to formulate a collective approach towards data strategy and EPR selection will yield efficiency and negotiating power with vendors. By collaborating on these crucial decisions, they can create a more integrated and interoperable healthcare system that benefits all stakeholders involved. This collective approach can not only reduce investment required in data strategy and EPR procurement but also enable an opportunity for cost savings through reuse of implementation and data migration capability. Once implemented, a more aligned system estate will facilitate data sharing, seamless information exchange, and lead to improved regional patient care outcomes.
Recommendation 2: guidance on levelling-up Trusts to HIMMS EMRAM level 5
An investigation comparing Trusts already at HIMMS EMRAM level 5 and above and those that are not who have the same system would enable NHS England to provide guidance, a to-do list and a roadmap for Trusts to help determine and action the gaps. If the gaps were understood and could be filled through better integration, architecture and use of data, perhaps by learning from successful practices elsewhere, there would be less need for some Trusts to feel they need to upgrade EPR systems to optimise decision-making processes, freeing-up cash for those who really need to invest in fundamental system transformation.
Recommendation 3: approach to business case development
We suggest the NHS adopt a modern approach to business case development, using a central template that is continually reviewed and updated in collaboration with Trusts and ICSs. With a cloud-based centrally hosted template and a copy for each Trust or ICS, NHS England would be able to continually compare and provide guidance and oversight. This approach may:
- speed-up business case process completion.
- ensure that a proper future home for data is considered at the same time as the decision over the future EPR.
- Ensure that Trusts and ICSs adopt NHS England's existing guidance on separating data from application.
Recommendation 4: Balancing functionality delivery between EPR and opensource, replicable Data Layer
In pursuit of advancing healthcare digitisation both for patient and hospital management, we suggest that Trusts and ICSs identify the desired functionality and assess the capabilities of EPRs already in place. They can identify the most cost-effective combination of extensions to the EPR or an EPR working alongside a well-integrated data layer from the point of view of initial investment, ongoing operational cost and digital and clinical innovation potential. EPRs are primarily architected for patient management and do not comprehensively address all aspects of Hospital management. Desired solutions to gaps in Hospital management are better serviced through bringing together HR, Estates, Finance and Operational throughput data.
Recommendation 5: Implementing an approach of minimum functional requirements to ensure equitable outcomes
In the context of varying levels of system maturity, convergence, and interoperability across ICSs, finding the right balance between EPR functionality and a replicable Data Layer becomes crucial. By carefully assessing the desired functionality and exploring the most cost-effective combination of EPR and data layer, a national body can enforce a minimum level of functional specification and Trusts and ICSs can align to these goals. Resulting outcomes at local level will become more equitable through a national lens. This approach empowers local healthcare organisations to maximise the potential of their digital and clinical innovation while optimising both initial investments and ongoing operational costs.
With national design coordination, NHS organisations can embark on this journey of maturation together, combining cutting-edge technology with strategic data management to build a stronger and more interconnected healthcare ecosystem.
Recommendation 6: Examine where data mesh v. data layer are the most appropriate option
Data Mesh is an architecture which allows for decentralised data ownership across systems and data products with strong central design governance. In this approach, individual teams or domains take responsibility for implementing common standards making data more accessible and manageable. This approach can be cost effective and prevent duplicate data storage where interfaces can be aligned in complex, dynamic environments. This might need vendors selling into the NHS to have signed-up to facilitate real-time data sharing.
On the other hand, a Data Layer refers to a centralised and standardised data infrastructure which stores pre-processed data from across an organisation, enforcing uniformity and consistency, optimising data structures ready for analytical, research and operational automation purposes. Bringing data together in an optimal data architecture for science and automation may well be a more cost-efficient solution long-term where legacy applications on legacy operating systems are otherwise having to be maintained or where a workforce’s technical developer skill is limited, and it helps if this is put in place for analysts.
Recommendation 7: disseminating best practice in Data Architecture and Platform set-up
NHS England could strengthen its dissemination of approved design artefacts as well as an improvement methodology in a roadmap via the central repository, the National Technology Resources for Integrated Care Systems, for the benefit of all Trusts and ICSs during their EPR selection, scoping and configuration stages. These artefacts might include:
- a common single patient view data architecture. This will enable a shared understanding of ambition, methodology and scope of data fields and metrics and their organisation to create a single patient view optimised for science and automation - a common need across all Trusts.
- essential considerations for and configuration details of cloud platform setups
- best practice cleansing scripts and machine learning matching routines which could then be used by each Trust going through the EPR implementation
- overarching guidance in a process flow (technology roadmap) of how to deliver the vision.
Common data architecture could be adopted in each Trust/ICS and sandboxes put in place for local extension and experimentation. Once proven such experimentation can be formalised into a newer version of the common data architecture. Essentially, the centre would be gradually encouraging a move towards a standard implementation of artefacts, with each ICS having a separate instance of the set of artefacts.
Recommendation 8: cultural change in emphasis
We suggest that NHS England could place more emphasis on coordinating and providing best practice from the centre, taking input from existing ICS implementations and leading Trusts, through the set-up of data architecture forums. As Trusts experiment and pilot extensions, we advocate sharing assessed benefits across all ICSs, thus moving towards standardised implementation of artifacts while maintaining the flexibility for unique instances and innovation. In this way, NHSE could provide top-down guidance, knowledge dissemination and prioritisation based on value delivered yet enabling vanguard ICS and Trust data teams’ autonomy.
Working Together for a Better Future
In this era of digital transformation, collaboration and building shared capability are paramount. NHS England has an incredible opportunity to foster a culture of innovation, open dialogue, and best practice sharing across the healthcare landscape. With a focus on providing cross ICS and Trust data strategy, by centralising validation and coordination of best-in-class designs and solutions, NHS England can accelerate all ICSs and Trusts in their journey towards a more mature and cost-efficient data infrastructure.
Let us come together and embrace this collective approach. As stakeholders, including Trusts, ICSs, and EPR vendors, we can collectively deliver substantial cost savings, improved decision-making, and enhanced patient outcomes. By working collaboratively and leveraging the insights and recommendations presented in this document, we can build a brighter future for healthcare digitisation in the NHS.
